Technologies, clinical reasoning and tissue stress
There is no question that technologies have added real value to clinical practice in terms of imaging modalities, gait analysis hardware and plantar pressure systems.
I have had access to various gait laboratories in my clinical career and continue to do so in my Research & Development role for Surgical Armoury where we are involved with a number of collaborative projects with different groups both within and outside of the Orthopaedic profession.
The key to the effective use of technologies is in defining the research or clinical question and designing the study accordingly.
Over the 20 years of using these systems it has been increasingly more obvious that the data we acquire from the process although objective in terms of data collection is still subjective in regard to its interpretation.
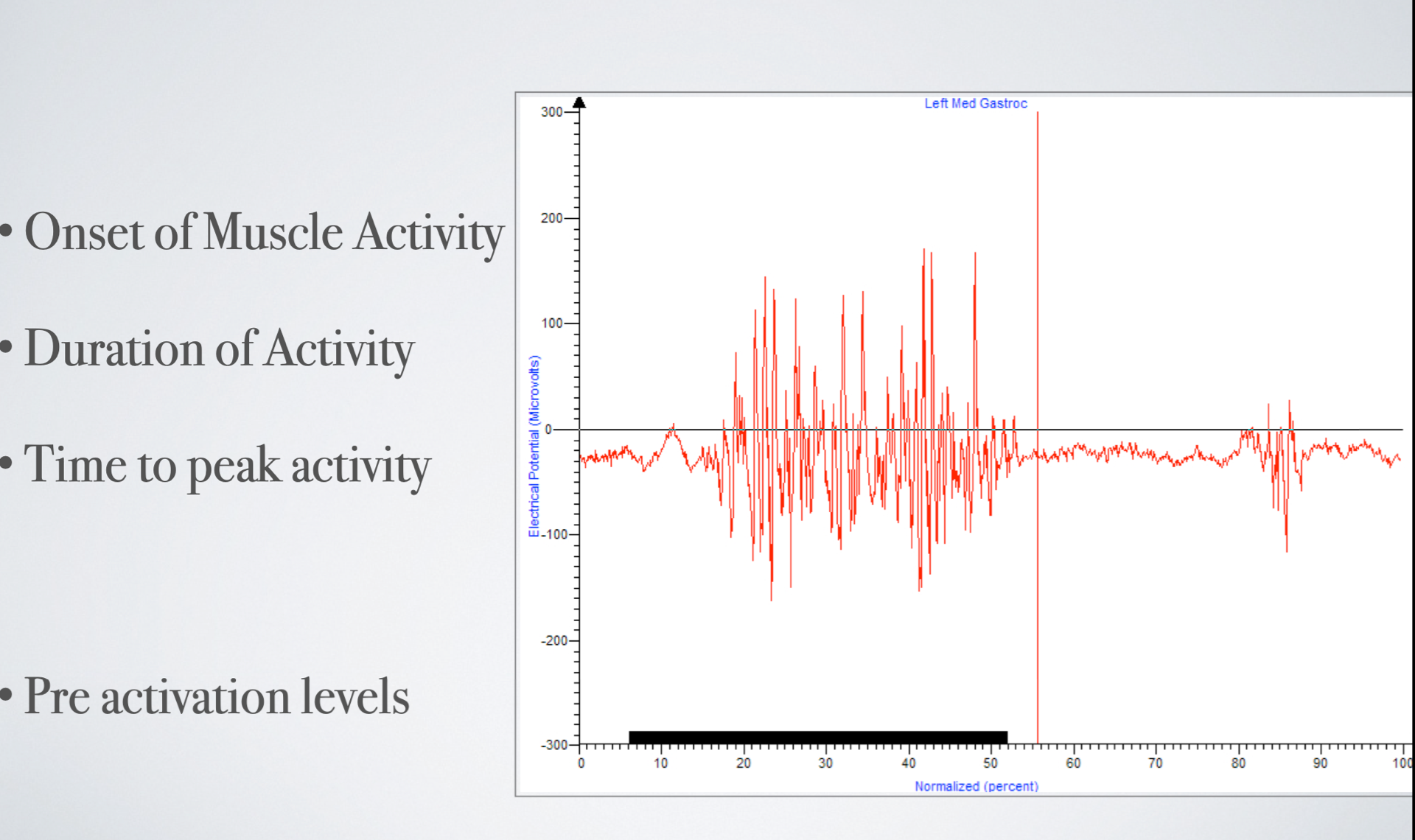
An example of this relates back to the work I undertook with a commercial company using surface electromyography (EMG) to assess the effect of footwear design.
The data (graph across) showed that the medial head of gastrocnemius and peroneus longus (stability and control mechanism muscle groups) were 30% less active in their pre activation phase when we compared the concept sandal against the market leader and my interpretation based on a physiological rationale was that over an extended period of time this would result in these 2 muscles been less fatigued than the same person in the alternative sandal.
I have stated many times to the various teams that I work with or the patient group that I choose to assess in this way that the systems allow me to add in an additional layer of objective support for the mechanical concepts that underpin my clinical reasoning.
This is the absolute crux of this blog, clinical reasoning is the foundation of clinical practice.
The use of technologies in obtaining an image of the foot has always been a fascinating area and one that I hope can be addressed. At the moment obtaining a scan of the foot is becoming more accessible and financially obtainable in clinical practice.
As a clinician and in my previous R&D roles I continue to review the scanning options when meeting with new or established foot scanning companies. The main limitation with these systems currently is not in the foot scan acquisition, you can obtain an excellent 3D model of a foot with an iPad and an additional piece of hardware, moreover it is in what happens beyond this point.


As with any orthotic process you must have a product at the end of this which reflects the foot shape that you are dealing with and there are too many times that the end product in no way reflects the foot I have been dealing with when I have trailled the scanning systems.
Similarly, when I have seen patients who have been unable to tolerate scanned produced orthoses there appears to be a significant difference on the profile of these orthoses compared against traditional bespoke process builds.
The image to the left is off a scanned built orthoses (left) vs a traditional build orthoses (right) for the same patient. You can see the arch profile is significatly different.
The image below on the left is the actual foot shape of the patient.
This is not the issue with the scanner, this is an issue with the hardware and software interaction and the algorithm process that is inherent to scanning systems, and until this is resolved I will continue with more traditional methods of gaining a foot model.
It is in the interests of the clinician to source efficient and cost effective ways of improving the orthotic manufacturing process but this should not be to the detriment of the patient and the end product supplied.
One of my concerns with the marketing of certain scanning systems is the apparent dumbing down of mechanical understanding with foot and ankle injury and the claim that the scanner and subsequent software and orthotic manufacture will meet these mechanical needs without the clinician been part of these decision making process.
Essentially, lots of systems offer the option of taking a foot model, pressing a button and have someone else, or an algorithm make the key choices on shell type, control features and modifications.
This is concerning, not only from a profession perspective but also on a medico-legal level as we need to be able to show sound rationale about the choices we make.
One of the recurrent themes that I hear from the different manufacturing groups that I have been involved with in terms of orthotic provision is the question from some clincians of ‘what should I do with this patient?” when the casts / foam box or scan had been shipped to the lab.
The whole essence of clinical reasoning is that if you are involved in providing an orthoses to a patient, you must be the one to make the key decisions on the orthotic design features, not a technician and not someone who has never seen your patient.
When I see my patient for the first time the key questions are formed around the key features of the tissue stress model;
Anatomically what structure hurts?
What is its assumed role in function?
Why is it this structure being overused?
What are the factors that I can influence to change the demand on this injured structure?
What other factors outside of internal forces do I need to influence
If I don't know what structure is compromised then I can not formulate an effective management plan that will help me deal with the presenting problem.
One of the best examples I often use is tibialis posterior tendinopathy. This video below is an example of a patient who had symptoms around the medial ankle area for 3 months and as you can see had a large range of rearfoot eversion and midtarsal joint rotation.
My thought process here is to see how much rearfoot eversion I can control and how much navicular drop / drift can I reduce.
If I can reduce these two movements then there is less mechanical stress on this tendon and the question of “what should I do with this patient?” has partly been answered for the orthotic intervention part of my management plan.
The type of orthotic design variables therefore relate to the shell stiffness that I want to use / what rearfoot control variables such as heel posting, medial heel skive, heel counter height are all a component part of my thinking.
I have not measured any joint relationships per se although at times I might try and quantify the degree of navicular drop / drift.
I do to want to block movement I just want to reduce the eccentric load and tensile stretch acting on the symptomatic tendon based on a sound physiological rationale.
Applying this tissue stress model as part of clinical reasoning skills I believe is key in understanding how you can bring value to our patient groups and also in designing orthotic design variables.
When I was asked to Chair the Biomechanics Summer School for LBG Medical I felt that we needed to explore this model in more depth and to try and illustrate how these concepts can significantly improve both our clinical reasoning skills and ultimately our patient outcomes and I believe that we put together a superb lecturing team from around the world that fulfilled that objective.
Mark Gallagher
Podiatrist
Share this post:

